Nigeria’s Federal Ministry of Health uses geospatial data to inform National Surgical, Obstetrics, Anaesthesia & Nursing Plan
An estimated five billion people worldwide do not have access to basic, safe surgical care. This disparity is particularly prevalent in sub-Saharan Africa, where obstetric complications, injuries, and cancer continue to cause significant morbidity, mortality, and long-term disability. In 2015, the World Health Assembly passed resolution 68:15, mandating countries to include emergency and essential surgical, obstetrics, and anesthesia care as an integral component of Universal Health Coverage. As a result, the Federal Ministry of Health of Nigeria (FMoH) set out to develop the Nigerian National Surgical, Obstetrics, Anesthesia and Nursing Plan (NSOANP) with the goal of helping millions of people in the country. The NSOANP will provide a realistic assessment of the state of emergency and essential surgical, obstetrics, and anesthesia care in Nigeria and lay out a clear roadmap for expanding access to these services.
To inform the NSOANP, the FMoH needed to understand the proportion of people in sub-Saharan Africa who can access, within two hours, a health facility that has capacity to perform caesarean deliveries, laparotomies, and treatment of open fractures (the bellwether procedures). However this information was not readily available. To obtain this data, FMoH mandated a baseline analysis of surgical access in Nigeria. In response, GRID3 mapped health facilities in Nigeria as well as visualised the surgical workforce in relation to population at the subnational level.
Analysing the state of surgical care in Nigeria
As a first step, the GRID3 Nigeria team estimated access to major regional and district hospitals based on travel time. These estimates were then used to assess the overall need for surgical resources at the country level with the assumption that only major regional and district hospitals can provide essential surgical care. Results indicated that the majority of the sub-Saharan African population (92.5%) reside in areas within two hours of a major hospital, based on spatially-defined travel times. Yet, 258-295 million people (115-132 million of whom are children under 15) lack access to safe surgery. Given the optimistic assumption of adequate surgical capacity of major hospitals, the true scale of the challenge of surgical disease is expected to be much greater.
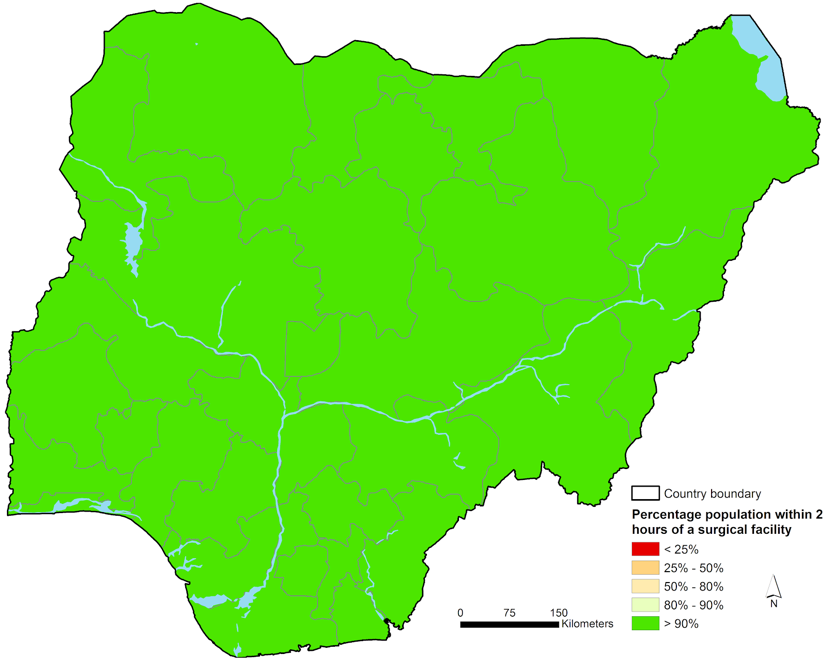
Once they mapped all health facilities, the GRID3 Nigeria team determined that the appropriate physical infrastructure for the delivery of surgical care may already exist: 90% of Nigerians lived within 30 minutes of a facility assumed to have capacity to provide safe surgical care, 98% lived within one hour of such facilities, and 100% within two hours.
Percentage of population within two hours of a surgical facility in Nigeria.
Source: Nigeria Federal Ministry of Health, 2019
As a final step, the GRID3 Nigeria team analysed FMoH’s data (at a highly aggregated federal state level) on the surgical and anesthesia workforce. Workforce data revealed inadequate availability of surgical and anesthesia personnel, with just 1.65 surgeons, anesthesiologists, and obstetricians (SAO), 100,000 people nationwide. The density of pediatric surgeons is even lower, at 0.14 per 100,000 children under 15. It is recommended that there be 20 SAOs and 1 pediatric surgeon per 100,000. When overlaid with GRID3 population estimates, the results also indicate a severe shortage of professionals required to provide surgical, obstetrics, anesthesia and nursing care.
Looking towards the future
Going forward, the NSOANP will be integrated into the National Strategic Health Development Plan and National Child Health Policy, ensuring that access to emergency and essential surgical, obstetrics, anesthesia, and nursing care is strengthened within the existing healthcare system. GRID3 will also use additional disaggregated data on Nigeria’s specialised medical workforce for a more refined analysis that will provide granular evidence for investments in the NSOANP.
Read the full report here.